One in five U.S. adults experienced mental illness in 2021. This represents 57.8 million people. However, only 47.2% of U.S. adults with mental illness received treatment in 2021.1 The country is deep in a behavioral health epidemic without enough providers to address the worsening crisis.
Because the magnitude of behavioral healthcare challenges is so great, and there is only so much that health systems can offer for preventative care, systems must collaborate with other experts and community partners. We examine new ways to take a proactive approach to behavioral health and describe the role of hospitals in that framework.
- Provider Shortage: As of September 2022, the
United States has a shortage of 7,871 psychiatrists.2
These numbers do not account for shortages of other behavioral
health providers such as clinical psychologists, Licensed Clinical
Social Workers, psychiatric nurse practitioners, and Licensed
Mental Health Counselors.
- Loneliness Worsening Due to the Pandemic: For
decades, Americans reported spending about 6.5 hours a week with
friends. But from 2014 to 2019, it suddenly dropped to four hours a
week. Not coincidentally, 2014 was the year smartphone ownership in
the U.S. surpassed 50%.3 The pandemic has no doubt
exacerbated loneliness: U.S. Surgeon General Dr. Vivek Murthy
raised the alarm about the devastating impact of the loneliness and
isolation epidemic in 2023. We watched our social networks wither
as we distanced ourselves for months on end.
- Unmet Social Needs Are Associated With Higher Self-Reported Rates of Behavioral Health Conditions: People with poor mental health were two times as likely to report an unmet basic need as those with good mental health, and four times as likely to have three or more unmet basic needs.4 58% of Gen Z reported two or more unmet social needs, compared with 16% of people from older generations.5
These perceived unmet social needs include:
- Income
- Employment
- Education
- Food
- Housing
- Transportation
- Social support
- Safety
Respondents reporting food insecurity are 2.4 times as likely to report multiple ER visits and twice as likely to report an inpatient visit over a 12-month period. Respondents reporting unmet transportation needs are 2.6 times as likely to report multiple ER visits and more than twice as likely to report an inpatient visit over a 12-month period.6
Given the provider shortage, what can health systems do to address existing behavioral healthcare treatment needs as well as prevent future ones from emerging due to unmet social needs?
The Role of the Hospital
As the highest acuity provider in the healthcare industry, hospitals have the power to change and direct how to care for the behavioral health population. While we are keenly aware of their current role in treating and stabilizing patients in the emergency room, hospitals need to change their approach to care as we move towards population health.
Instead, health systems need to implement a structure that adequately connects patients to the resources they need through their community partners and employ a strong case management team to ensure the patients are following through with partner referrals. This will require investment in case managers to periodically follow up with patients and support from ancillary departments like quality management to ensure that hospital partners stay aligned with the health system's standards of care.
As reimbursement shifts towards global payments and away from fee-for-service, health systems may also be incentivized to financially support their partners to keep patients out of the emergency room and inpatient environment.
Citizen Advocates: A Model for Behavioral Health Treatment and Prevention
Citizen Advocates is a New York nonprofit that provides a full range of intellectual/developmental disability, mental health, and addiction prevention, treatment, and recovery services in addition to support that promotes individual health through stable housing, job training, transportation, and more. Its CEO, James Button, has extensive experience in transitioning from fee-for-service to risk-bearing contracts with managed care companies.7 Citizen Advocates is unique in that it is a standalone organization serving several largely rural counties across Northern New York that is addressing basic needs as part of behavioral healthcare.
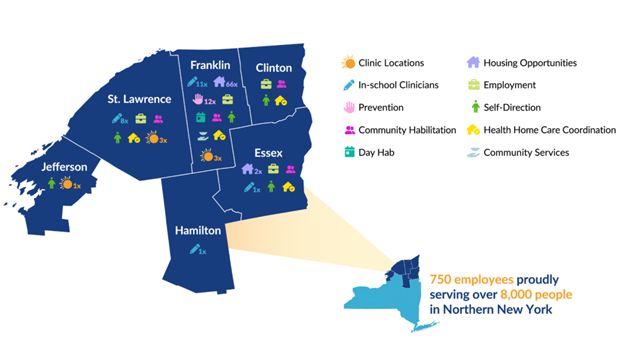
Image Source: Behavior & Mental Health Services | NY | Citizen Advocates
- Immediate Treatment: Because a behavioral health crisis rarely happens during normal business hours, Citizen Advocates has recently opened its third Behavioral Health Urgent Care Center to provide 24/7 mental health and addiction services. It was designed to fill a gap in the healthcare system by providing an alternative to the emergency department for individuals who need urgent, more specialized care in a safe, home-like environment. This personalized, one-on-one care can lead to better outcomes and is generally less costly than hospitalization.
The facility offers:
- Medication management
- Adult and pediatric stabilization care
- Individual, group, and family mental health & addiction counseling
- Peer support services
- Care coordination
- Smoking cessation
- Access to services via telehealth
The organization's original and first Behavioral Health Urgent Care Center was recently relocated in 2023. The revitalized building was renovated for $2.2 million and staffs 34 employees, including physicians, psychiatric mental health nurse practitioners, nurses, therapists, case managers, peer specialists, and customer support.8
- Prevention: Citizen Advocates has youth
prevention and education specialists stationed in roughly a dozen
Northern New York schools. Prevention specialists work with
teachers, counselors, and administrators to develop trusted
relationships with students, increase awareness around risky
behaviors, and support referrals for struggling students. The
program reinforces knowledge, coping skills, prevention techniques,
and interventions to support healthy choices when it comes to
addiction, bullying, mental health, and promoting
self-care.9
- Housing Stability: Citizen Advocates replaced several blighted properties with a mixed-use development that will offer safe, stable, and affordable housing in the heart of downtown Malone, NY. Referred to as the Harison Place project, there are 40 affordable and supported living apartments above five commercial spaces located on the ground floor. Residents will have access to mental health and addiction services, career and training support, tenant education, financial planning and literacy, life skills, healthcare coordination, and more. The project was designed to help homeless or housing-insecure individuals and families get back on their feet. The project was funded by an assortment of government and nonprofit agencies, including $7.8 million in Low Income Housing Tax Credit Equity, $3.8 million from the NYS Homes and Community Renewal, and $900,000 from the Rural and Urban Community Investment Fund. The New York State Energy Research and Development Authority (NYSERDA) provided $40,000 in support and the Office of Temporary and Disability Assistance also provided $4.8 million from the Homeless Housing and Assistance Program. Citizen Advocates provided $4.2 million to fund the project and the Federal Home Loan Bank provided $600,000.10,11
Citizen Advocates fills many other social need gaps such as providing food to children during the summer,12 help with transportation to medical appointments, job search assistance, along with residential and day programs for individuals with intellectual and developmental disabilities. These are all designed to help all individuals live a life of their choosing, wherever that may be.
What Could the Citizen Advocates Approach Look Like in Your Community?
Let us apply the Citizen Advocates model to the Charlotte, NC metro as a hypothetical test case. Citizen Advocates' 750 staff members serve a population of roughly 394,000 people. Applying this same ratio of roughly 19 employees per 10,000 residents, "Citizen Advocates" replicated in Charlotte would need 5,000 employees. For size comparison, this is approximately the same number of employees at LPL Financial, a large financial services firm headquartered there. While this scenario may sound unrealistic, it speaks volumes to the investment and resources required to treat this population, and most notably speaks to how health systems need partners in the community to comprehensively address the behavioral health crisis.
HEART Program: A Mobile Response Behavioral Health Team
Another community behavioral healthcare model is the HEART Program in Durham, North Carolina, which stands for "Holistic, Empathetic, Assistance Response Teams." The city-funded program was launched in June of 2022 and sends social workers or peer support specialists to behavioral-health-related calls, instead of the police. It has 50 employees and has recently expanded its schedule to 12 hours a day, 365 days a year. It diverts 911 calls from the law enforcement department to enable them to focus more on criminal activity.
It categorizes services into the following programs:
- Crisis Call Diversion (CCD): CCD embeds mental health clinicians in Durham's 911 call center.
- Community Response Teams (CRT): CRT dispatches unarmed 3-person teams as first responders to non-violent behavioral health and quality of life calls for service.
- Care Navigation (CN): Care Navigators follow up with people after meeting with one of our first responders to help connect to the community-based care they need and want.
- Co-Response (CoR): CoR pairs clinicians with Durham police officers to respond to certain calls for service that pose a greater potential safety risk.
According to its dashboard, HEART has responded to 7,860 cases in the last 12 months. Dashboard users can view response locations on an interactive map by program type or by day of week/hour of day.
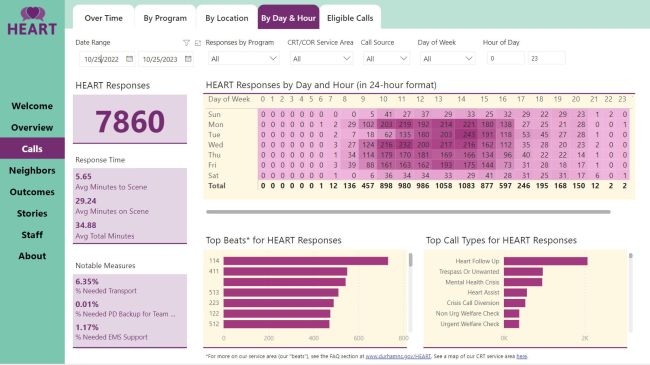
Link: www.durhamnc.gov/HEART-data, accessed 10/25/2023
With a starting annual budget of $4.1 million to cover a third of the city for about half the day, it was recently expanded to a budget of $6.4 million to offer citywide coverage for at least 12 hours per day. The full increase would allow them to triple their call volume to 13,600 calls per year, which equates to 10% of all 911 calls.13
The program was incubated by Harvard Kennedy School's Government Performance Lab through its Alternative 911 Emergency Response program, which has helped 17 jurisdictions, including Durham, establish programs in the last two years.14
What Could the HEART Approach Look Like in Your Community?
In our experience, the cost to treat a patient in the emergency room often exceeds $600 per hour. Behavioral health patients typically have an emergency room length of stay exceeding six hours and, not uncommonly, multi-day stays when trying to find appropriate inpatient placement. Localizing this cost in our Charlotte, NC metro example equates to almost $500m in behavioral health emergency department costs annually. If a mobile response unit could help health systems divert even a conservative 10% of their behavioral health emergency department volume, in the Charlotte metro, it would save health systems $50m in a single year. The $50M savings is almost 8x greater than the $6.4M to fund the current Durham HEART program. As healthcare reimbursement shifts away from fee-for-service, our health systems will have even more incentive to fund and support partners like HEART and Citizen Advocates.
The Community Approach
The behavioral health crisis is big and real and it is not going away. For our clients and communities, programs like the HEART model are low-hanging fruit, but the Citizen Advocates model is the gold standard starting point for truly tackling this crisis head-on. As described in our examples above, there is a strong business case for health systems to support these programs financially and through patient referrals. As the old adage goes, "It takes a village to raise a child," it will take an entire community of healthcare providers, educators, family, and friends to address behavioral health.
Footnotes
1. Mental Health By the Numbers | NAMI: National Alliance on Mental Illness
2. Mental Health Care Health Professional Shortage Areas (HPSAs) | KFF
3. Opinion | Americans are spending more time alone. Let's reverse that. - The Washington Post
4. Patients struggle with social determinants of health: medical providers can help | McKinsey
5. 6 ways Gen Z interacts differently with the healthcare system (beckershospitalreview.com)
6. 20190415_SDoH_Infographic_VF.18 DF (mckinsey.com)
7. Behavior & Mental Health Services | NY | Citizen Advocates
8. https://citizenadvocates.net/blog/citizen-advocates-celebrates-new-name-and-new-home-for-24-7-care/
9. https://citizenadvocates.net/blog/prevention-program-lessons-resonate-beyond-graduation/
10. https://citizenadvocates.net/blog/citizen-advocates-breaks-ground-for-harison-place-project/
11. https://citizenadvocates.net/community-housing-living/
12. https://citizenadvocates.net/blog/keeping-youth-fueled-for-healthy-summer-fun/
13. https://www.newsobserver.com/news/local/crime/article280898288.html#storylink=cpy
14. https://govlab.hks.harvard.edu/alternative-911-emergency-response
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.

