Unprecedented demand for Urgent and Emergency Care Services
According to new research from the Red Cross, slightly less than 1% of the population of England attend A&E at least five times a year. As a group, these individuals account for approximately 16% of all A&E attendances and 26% of all hospital admissions in England. A large proportion of these 'frequent attenders' have one or more long-term, life-limiting condition. The research shows that mortality rates amongst individuals within this cohort aged between 30 and 49, are approximately 7.5 times higher than amongst individuals of the same age in England in general.
Developing a 'Covid-recovery' Virtual Ward Service
At present, recovery processes in the NHS are being hampered by a lack of capacity in acute settings driven in part by high and rising demand for Urgent and Emergency Care. Peopletoo have been working with a number of localities/ places to support them in responding positively to the challenges (across health and care) posed by both the ongoing Covid pandemic and recovery efforts.
Peopletoo have developed, with a locality in the North of England, a "Covid recovery" Virtual Ward service, which aims to reduce the demand for non-elective care amongst the highest frequency users of these services. The design of the service builds on the original "Croydon" Virtual Ward model, developed in 2005 and the learnings from variations on this model used in Devon (2009/10), Wandsworth (2009/10) and Harrow (2018/19). Whilst the outcomes delivered by the model variants differ, there is strong evidence that Virtual Wards provide a safe, cost -effective alternative to an acute admission, through a package of primarily community based-resources.
The overarching model and its components
The "Covid recovery" Virtual Ward model we designed, has a number of differences from the service introduced in primary care in Croydon in 2005, however it retains the core features of:
- A predictive model to identify individual patients at high risk of an A&E admission
- A multidisciplinary approach to enabling case management at home, using a structure, processes and systems akin to a hospital ward.
The overarching model (with its additional elements) can be summarised as shown below.
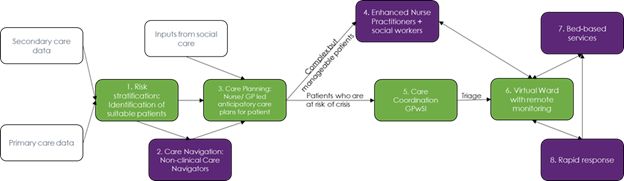
The key components of the model can be described as follows:
- Primary and secondary care data is used to identify suitable individual patients who correspond to high-usage patient segments. Most virtual ward variants focus on individuals aged 65+ with one or more Long-term Condition, however current system pressures highlight the need to broaden eligibility to working age adults with complex needs.
- Individuals who correspond to a high-usage patient segment but do not yet, have an urgent need for the Virtual Ward service, could be provided with care co-ordination services provided by non-clinical Care Navigators. Care Navigators will be able to expedite the admission of these patients into the Virtual Ward if needed.
- Individuals adjudged to have an urgent need for Virtual Ward services, either following step 1 or step 2, will be referred to Care Planning to enable the creation of an Anticipatory Care Plan.
- Individuals from step 3 adjudged to have complex needs which can be managed effectively outside the virtual ward, will be referred to a team of Enhanced Nurse Practitioners working with Social Workers to provide non-urgent, home-based support/ when needed.
- Individuals from step 3, who the Anticipatory Care Plan adjudges are potentially in crisis, will be referred to a Care Coordination service run by GPs with a Special Interest, aligned to the needs of the patient's population segment e.g. diabetology, gerontology etc.
- From step 5, the GPwSI will triage the patient, referring them to the Virtual Ward with remote monitoring if this is the best solution. Whilst on the Virtual Ward, patients' cases will be discussed with a Multi-disciplinary Team comprising e.g. Social Workers, Occupational Therapists, Community Pharmacists, Gerontologists, Psychiatrists, GPs, Voluntary Sector Workers etc. on a weekly basis, with Care Navigators responsible for coordinating the delivery of their care.
- Virtual Ward patients requiring a step-up bed following crisis can be referred into bed-based services. Similarly, patients discharged from hospital into the Virtual Ward may need step-down provision.
- A Rapid Response service will be available to support patients in managing crises in their own home; where required the service can escalate to an ambulance call-out, or refer into the Virtual Ward's bed base or other bed-based services (Acute/ community) as needed.
System-level benefits Anticipated
Evaluation of a similar Virtual Ward model demonstrated that admission to the virtual ward lowered demand for Urgent and Emergency Care services amongst participants in the 6 months following discharge, translating to:
- 40% reduction in GP usage,
- 86% reduction in 111 calls
- 50% reduction in A&E attendances
- 79% in NEL admissions
Delivering similar outcomes across English systems/ localities (places) would result in substantial savings in relation to demand management and large increases in capacity to support Covid recovery processes.
Patient-level benefits Anticipated
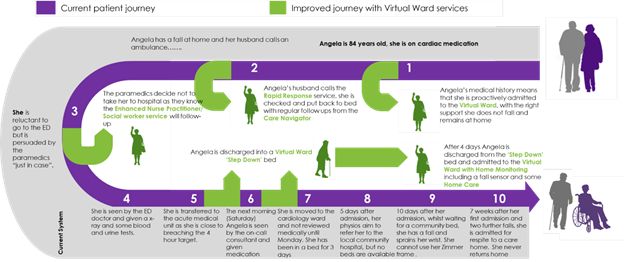
Angela's story (below) demonstrates how the Virtual Ward service proposed could transform patient outcomes. In this particular example, the Virtual Ward would deliver savings between £1.5k and £19.5k, per incident, depending on the point of intervention.
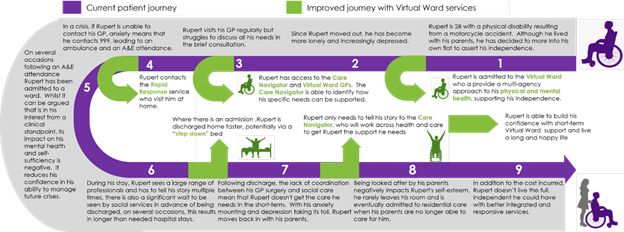
Rupert's story demonstrates how the Virtual Ward service proposed could deliver savings between £1.5k and £32k over the course of a year.
Finding out more
Peopletoo are eager to work with systems and localities to develop business cases which outline the cost effectiveness and efficacy of a locally configured, Covid-recovery Virtual Ward model. We have developed approaches to:
- Determine, on the basis of community resources currently available, the cost of implementing and running the service
- Quantify the likely cost-saving of implementing the Covid-recovery Virtual Ward service vs. the cost of implementation
- Calculate the likely volume and value, of the acute resources that will be freed-up as a result of improved demand management.
Originally published 1 December 2021
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.
