Despite high standards of cancer care in the UK, diagnosis is sometimes delayed. Doctors may miss symptoms, fail to follow referral guidelines or make mistakes in interpreting x-rays, scans and biopsy samples.
Claims for damages after such delays are complex. Patients need to show negligence. But they also need to show the mistake has caused harm. This can be difficult in cancer claims. How do you show what stage a cancer had reached at a time when no one diagnosed it? If no investigations were done, what evidence can you rely on?
Delayed diagnosis: what did the cancer look like when no one saw it?
Without direct evidence, experts may have to work on two sources of information: what they know about the cancer when it was diagnosed; and what we know about how quickly cancers of that type develop. They then have to 'back-calculate' to work out what stage a cancer had reached at a previous point in time.
Usually the first issue is relatively straightforward. X-rays and scans can tell us about the cancer's size, exactly where it is and how far it has invaded other structures. Tissue samples from biopsies, analysed under the microscope, give information about the cancer's cells. This helps identify the type of cancer and how it behaves.
The second issue is much more complex. When people are diagnosed with cancer they are generally treated. Researchers do not just watch how cancers progress in untreated patients. This means that good data on how cancers develop untreated may not exist. Experts often have to piece together information from limited sources. Because the data is limited and may be open to different interpretations, this is an area where experts often disagree. Many clinical negligence cases turn not on whether a mistake was made but whether it caused harm.
How are cancers staged?
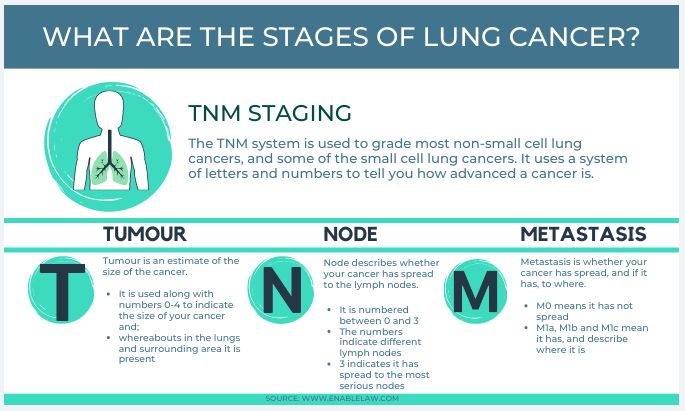
Experts classify cancers by 'stage'. 'Stage' refers to how far a cancer has progressed. For many cancers, the staging system looks at 3 factors. The first is the size of the tumour and whether it has invaded other structures (T). The second is whether it has spread to the lymph nodes (N). The third is whether it has spread further afield or 'metastasized' (M). So T1 will normally be a small, early stage tumour which has not invaded local tissues; T4 will be larger and invasive. N0 is not found in lymph nodes; N1 will be found in local lymph nodes and N2 will have invaded more. M0 is a cancer which has not spread to other organs (brain, lung, liver and sometimes bone); M3 has spread to a number of sites.
Cancers are also classed by grade, which indicates how aggressively they behave.
How do the courts deal with claims?
A recent case assessed the merits of different approaches to causation1. It may make it easier to understand the approach courts will take to similar cases in the future.
On 22 May 2016 Kevin King underwent a chest x-ray at James Cook University Hospital. It showed an abnormality which had not been there previously. Nothing was done to investigate. 6 months later, a further chest x-ray on 25 November 2016 showed that the suspicious finding had increased in size. He was diagnosed with lung cancer. By then, the cancer at the primary site in his lung had spread and there was a secondary tumour in his subcarina (an area between the bronchi and below the trachea). He was treated with chemotherapy but died on 2 February 2017.
His estate brought a claim in negligence against the Hospital Trust responsible for his care. It alleged that but for a breach of duty in failing to investigate in May and June 2016 Mr King would have been successfully treated and survived.
The Trust admitted breach of duty but denied that earlier treatment would have made a difference to the outcome.
At the trial, the judge heard evidence from oncologists for both parties. They agreed on several points: this was a squamous cell lung cancer; in June 2016 it was about 3 cm in size; its 'T' stage was either 1 or 2 (depending on whether it was 2 to £ cm or 3 to 4 cm); and there were no metastases (M0). Where they disagreed was whether it had by then spread to the lymph. The Claimant's expert, Dr Lester, thought not – the tumour should be categorised N0 and using a different staging system that was be 1A3 or IB. The Defendant's expert, Dr Peake, thought the mediastinal and/or subcarinal nodes were involved and that it was N2. It should be classed as Stage 3A.
Dr Lester thought Mr King would have lived for 8 years from the date of surgery – until June 2024. Dr Peake's view thought he would have lived only 29 months – to November 2018.
The case therefore turned on whether lymph nodes were involved in June 2016. The judge accepted Dr Lester's evidence and the Claimant won. It is helpful to look at which arguments found favour.
Four arguments
1 – Statistics: how many early stage cancers have spread?
The first argument was based on statistics for the number of T1 or T2 tumours which are in fact found to have spread to the lymph. There were 2 key research papers, one led by Oda and the other by Goldstraw. Oda's paper concluded that it was only 23.6%. Goldstraw's had separate figures for T1 and T2 cancers. For T1 it was 19.6% and for T2 it was 32%. The evidence of both papers made it more likely than not (more than 50% likely) that Mr King's cancer had not in fact spread. So earlier management would have made his survival likely.
Dr Peake nevertheless thought Mr King would have been in the minority whose cancer had in fact spread. His put forward several arguments in an attempt to establish why. None of them persuaded the judge.
2 – How long Mr King actually lived
The second approach started from the fact that Mr King in fact survived 8 months from the missed diagnosis. Both experts drew conclusions from this as to how advanced his disease must have been.
The research here was led by Wao. This was a meta-analysis. In other words it reviewed a number of existing research papers. It assembled data as too how long people survived without treatment. The average for stage 1 and 2 disease was 12 months. For stage 3 and 4 it was 5.03 months. So was Mr King's 8 month survival more like stage 1 and 2 on the one hand or 3 and 4 on the other?
Unlike the patients in the study, Mr King had undergone some treatment. His was treated with chemotherapy, which is toxic and may have contributed to his death. Dr Lester also thought that by the time of diagnosis he was already in worse health than other patients in the study. Both these factors meant he was less likely to live as long as the average for reasons other than the stage of his cancer. His 8 months of survival was therefore more like 12 month survival in healthier patients with early stage cancer than 5.03 month survival for patients in later stages.
Dr Peake disagreed. He did not think Mr King was in particularly poor health or that the impact of chemotherapy was clear. He thought 8 month survival suggested his cancer was already at a late stage in June 2016.
The judge was not persuaded by these arguments: the evidence here was too uncertain to make any finding one way or the other.
3 – How quickly do secondary tumours grow?
The third argument was based the size of the secondary tumour in his subcarinal and its likely growth rate. By December 2016 it measured 5 x 3.5cm. The primary tumour measured 4.5 x 3 cm. Dr Peake argued that, because of what we know about the speed at which secondary tumours grow, it must have already been there in June 2016.
Arguments about how fast secondary tumours grow are often highly contentious although they are often raised in clinical negligence claims. There is some evidence as to how long it takes for a primary tumour to double in volume – its 'doubling time' (a single cell divides in 2, then 4, then 8 etc). However, this is not always clear. There may be periods when tumours double a constant rate but other times when they grow more quickly or more slowly. Some tumours are thought to grow along a Gompertzian (S shaped) curve – slow initially, then rapidly, then slowly again.
Less is known about the growth rates of secondary tumours but they may well grow much more quickly than primaries.
In Mr King's case, the primary tumour was thought to have a doubled in volume over about 117 days. Dr Peake argued – based on a research paper by Wang and others – that the secondary cancer would have grown at a similar rate, meaning that it would already have been there in June 2016. Dr Lester criticised that view and the judge rejected it. There were a number of flaws in assuming secondary cancers grow at the same rate as primary cancers. They may start not from one cell which divides, but as a cluster of cells, developing at a faster rate. Further, nodal disease may start as several lymph nodes aggregating to form one mass. In any event the size of the group of patients studied by Wang was too small to provide reliable data and the paper did not in fact support the conclusions Dr Peake claimed.
4 – Clinical experience
The final argument was based on the clinical experience. Dr Peake said that in his experience of treating hundreds of patients, he did not recall nodal disease progressed from nothing to the size of this secondary tumour within such a short period.
There is a place for evidence based on experience, rather than research, particularly where research evidence simply does not exist. However, where there is better evidence, it is unlikely to be compelling.
Again, the judge was not persuaded. He looked at the experience of the experts. Dr Lester was a leader in the field of lung cancer. Dr Peake had more years of experience but saw fewer lung cancer patients than Dr Lester. Lung cancer stopped being one of his main interests in 2011 and he had stopped treating lung cancer in 2015. There was no reason to credit Dr Peake's experience over that of Dr Lester. Generally, the judge favoured Dr Lester's evidence.
Conclusion
Claims for damages after the delayed diagnosis of cancer are notoriously complex. There is often disagreement as to what extent the delay actually caused harm, if at all. The arguments raised in Mr King's case are common ones. What is particularly helpful about the judgment is the careful scrutiny given to 4 different approaches. Only one was found to have merit, and that was a statistical argument based on the number of early stage cancers which have already spread to the lymph. With this particular type of cancer, the research showed that it spread early only in a minority of cases. It was unlikely that it would have done, therefore, in Mr King's case.
This should help patients in a similar situation and make it more difficult for claims to be defended on the common basis that, for one reason or another, the patient falls within the minority rather than the majority. It therefore provides a helpful indication of how the approach the court is likely to take, and the sort of evidence which will prevail, in future cases.
Footnote
1 Tracey King v South Tees NHS Hospital Foundation Trust [2020] EWHC 416 (QB)
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.
