This report was co-authored with the American Medical Association.
Background
Three years following the onset of the COVID-19 public health emergency (PHE), states across the United States continue to enact permanent changes to telehealth laws that impact how physicians and other health care professionals can deliver care remotely. Nearly all states issued temporary policy flexibilities to swiftly expand access to telehealth at the onset of the PHE that accelerated the implementation, adoption, and widespread use of telehealth across the health care industry.1 Telehealth has become embedded in the practice of medicine, with patients and physicians alike overwhelmingly in support of care via telehealth.2,3 Starting in 2021, states shifted focus from temporary policy implementation toward assessing which pandemic-era policies should be continued on a permanent basis to support ongoing access to telehealth in a manner that meets the standard of care.
The American Medical Association (AMA), with its commitment to ensuring equitable and accessible telehealth services, has been closely tracking state legislative activity related to telehealth throughout 2023. Tracking efforts indicate that states generated the most legislative activity around the following telehealth policy trends:
- Coverage and payment parity
- Telehealth licensure
- Audio-only telehealth
- Medication abortion via telehealth
This report aims to provide a year-end snapshot of the current state of these policy trends, including an overview of each issue and a summary of 2023 legislative activity with examples of passed legislation.
Key legislative trends in telehealth, 2023
Coverage and payment parity
Overview: "Coverage parity" requires payors to cover a service via telehealth if it is also covered in-person and can be delivered remotely while meeting the standard of care. "Payment parity" requires payors to reimburse for telehealth at the same rate as the equivalent in-person service. Coverage and payment parity requirements are most frequently codified in state laws that outline coverage and reimbursement requirements for payors. These laws, and specifically coverage and payment parity, have enabled physicians to invest in new technologies and fully implement telehealth in their practice. The AMA considers fair and equitable coverage and reimbursement for telehealth services as essential to supporting implementation across the physician community and enabling access to care for all patient populations.
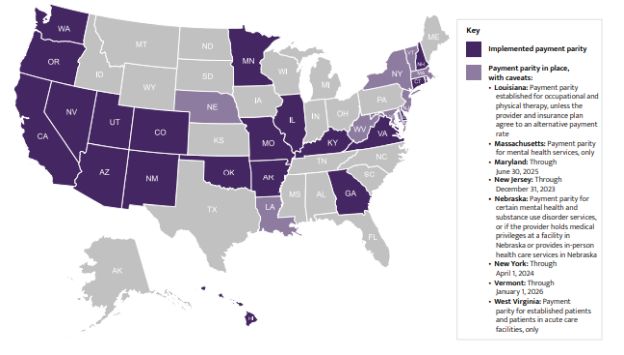
Coverage parity has been widely adopted across the United States—at the start of 2023, more than 40 states required payors to implement coverage parity.4 While there is broad support for coverage parity across the United States, many states are still considering how to appropriately pay for telehealth in light of a lack of robust data as to whether telehealth services cost more or less to deliver than in-person services. By January 2023, more than 25 states had implemented payment parity; 21 states had implemented permanent payment parity, while five had implemented payment parity with caveats (e.g., temporary implementation with a sunset date; applied only to specific services, such as behavioral health).5
Legislative activity and state examples: There was minimal legislative activity in 2023 aimed at coverage parity as it was previously adopted by most states. A handful of states introduced legislation that included coverage parity language aimed a specific payors, but none were passed (e.g., North Dakota introduced Senate Bill 2160, which would establish coverage parity for public employee benefits; Michigan introduced House Bill 4579, which would establish coverage parity for state-regulated commercial plans).
Three states passed new payment parity requirements this year:
- Colorado passed House Bill 1088, which established permanent payment parity for behavioral health services delivered via telehealth to Veterans.
- Hawaii passed House Bill 907, which, in addition to many other changes, required payment parity for services delivered through "interactive telecommunications systems,"6 and established that audio-only services "for the purposes of diagnosis, evaluation, or treatment of a mental health disorder" will be reimbursed at 80% of comparable in-person rates through December 31, 2025.
- Nevada passed Senate Bill 119, which implemented telehealth payment parity under certain circumstances, including when the services: (1) are delivered to patients located in rural areas or are furnished by certain health care facilities (i.e., federally qualified health centers) and are not via audioonly, or (2) are for behavioral health (e.g., mental health and substance use disorder) counseling or treatment, including when the services are delivered via audio-only. Through 2024, originating sites also include the patient's home.
As of October 2023, 21 states have implemented policies requiring payment parity, eight states have parity in place with caveats (e.g., temporary parity, applied to select service types) and 21 states have no payment parity.7
FIGURE 1. Map of states with laws requiring insurers to implement telehealth payment parity8 (as of October 2023)
To view the full article, click here.
Footnotes
1. Manatt Health, "Executive Summary: Tracking Telehealth Changes State-by-State in Res ponse to COVID-19" (accessed October 2023)
2. AMA, AMA digital health care 2022 study findings (accessed October 2023)
3. JD Power, "Telehealth Emerges as Preferred Channel for Routine Care While Increasing Access to Mental Health Treatment" (accessed October 2023)
4. Center for Connected Health Policy, Policy Finder: Parity (accessed December 2022)
5. Manatt Health, "Executive Summary: Tracking Telehealth Changes State-by-State in Response to COVID-19" (accessed December 2022)
6. Hawaii defines an "interactive telecommunications system" as, at a minimum, audio and video, with the exception of mental health services, which may be covered and reimbursed if conducted via audio-only.
7. Manatt Health, "Executive Summary: Tracking Telehealth Changes State-by-State in Response to COVID-19" (accessed October 2023)
8. For the purposes of this map, telehealth payment parity refers to video visits.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.



